Biosimilars Become an Increasingly
Important Part of Pharmacy Care
During the past year, there has been a lot of buzz about biosimilars as lower-cost alternatives to biologic drugs. Biosimilars are biologic medications that are highly similar to drugs already approved by the FDA. They are used for treating the same conditions and have the same mechanism of action as the reference, or originator, products. Through clinical trials, biosimilars have been proven to be just as safe and effective as their reference biologic drugs, meeting the same quality standards.
There is a growing expectation that biosimilars will transform the specialty drug landscape just like generic drugs did for traditional medications. They can increase access to important therapies and improve patient outcomes, all while providing a lower-cost option for patients.
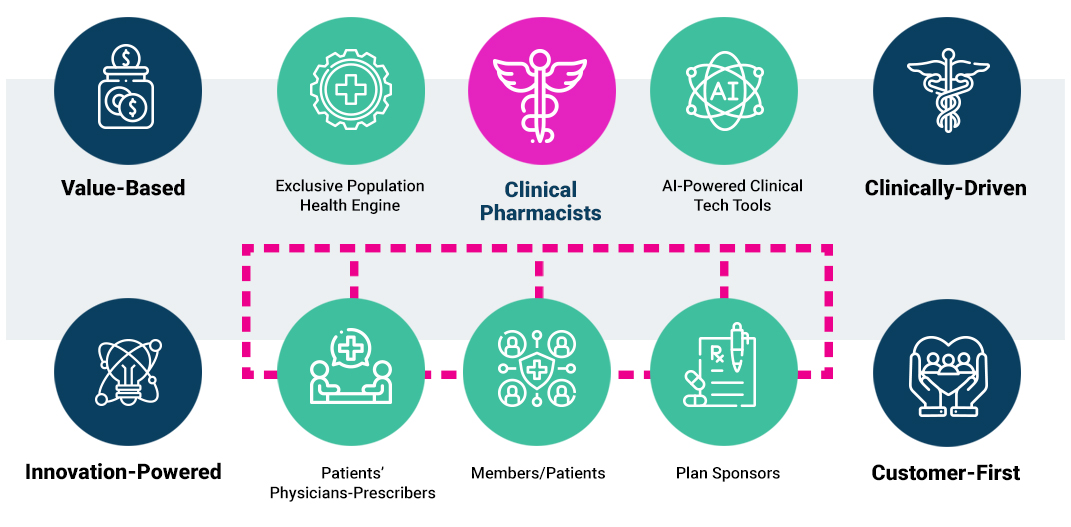
As the leading clinically-driven PBM company, EmpiRx Health has been an early adopter of biosimilars. Why? Because biosimilars offer the same level of safety and effectiveness as the original products, but at a lower cost – sometimes substantially lower. In fact, EmpiRx Health was one of the first PBMs that started to prefer lower cost biosimilars to original products.
Many other PBM companies are not prioritizing the lower cost biosimilars because doing so would run counter to their business models. These legacy PBM business models are fundamentally misaligned with the needs and interests of plan sponsors and their members.
In early 2023, EmpiRx Health was the only PBM that decided to prefer the lower cost Humira biosimilars in its formularies. Prior to making this decision, EmpiRx Health’s pharmacy experts performed a thorough review of available clinical data, dosing and formulation options, and other critical factors impacting member experience. Following that comprehensive review and analysis, we decided to select two of the lowest priced Humira biosimilars for our formulary.
This Humira formulary decision was consistent with our clinically-driven, customer-first pharmacy care approach, which puts the pharmacist at the center of the care model. When you put the pharmacist back in pharmacy benefits management, everyone wins.